|
| My boys on their new trampoline |
The visit with the plastic surgeon went well and they were able to remove the stitches. They really did a number on my neck this time and I don't think having the stitches in for three weeks did me any favors. The stitches came out easy enough and other than it taking an hour longer than it should have, the visit was uneventful.
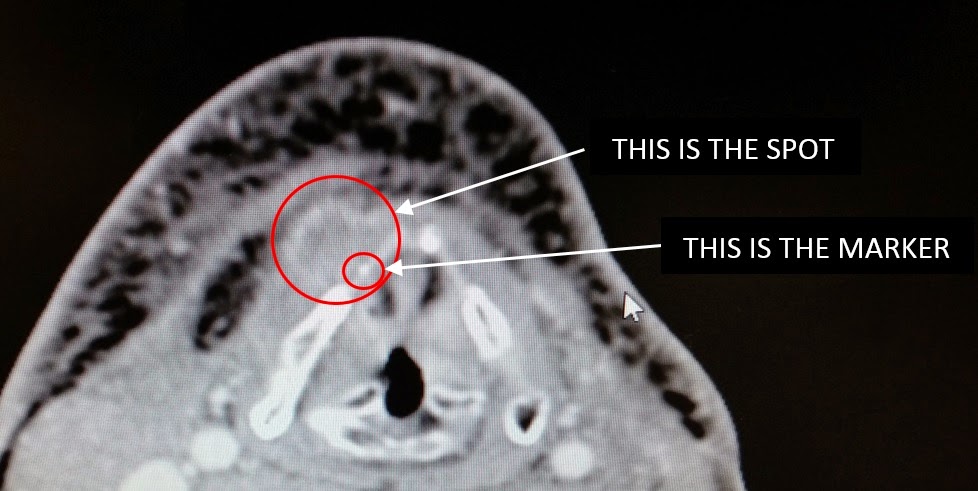
From the medical center, we raced out to the Memorial City office to meet with my ENT surgeon. This was our first visit to this office and it took some time to find it, but we made it and the entire visit didn't take too long. Overall, the visit was good. I got to talk with the surgeon and her PA, both of which I have known for too long now. My surgeon reiterated how good she feels about the outcome of the surgery and the results of the pathology that we got back recently. She always likes to give me warnings that I usually just shrug off but this time she actually chuckled a little and said "you aren't going to listen to me at all, are you?" as she gave me some of her guidelines on what I should and should not eat. She talked a little about me being near water and I held my hand to my upper chest and said I would only get in the water that deep, to which she held her hand at her knee and recommended that I not get in deeper than that. Somewhere in between is probably where I will end up, although I don't have to worry about that for a while. I found out also that the voice prosthesis is not a done deal yet. They need to see in the next CT scan results what the inside of my neck actually looks like and where everything is in order to know if they can punch the hole or not. The problem is my pectoral flap that they moved and stretched in this procedure and it's location relative to the spot where they will have to punch the hole between my trachea and esophagus. If it is in the way, I might not be able to have the prosthesis, but we will have to wait and see. My official followup plan is to have a CT scan roughly 8 weeks out from surgery. That will be the new baseline and will tell them more about the TEP procedure that I can hopefully have. After the baseline CT, I will have a CT every 3 months to look for new tumor growth or trouble spots. Other than that, it is just rest and recover.
Still trying to get used to my inability to speak. I get frustrated very easily. Very, very easily. I hate the electrolarynx, but I guess I need to get some practice with it. I am reading a lot about esophageal speech, but it appears to be tough to master and take a long time to get good at. There are options, but nothing will happen overnight. I need to start doing some physical therapy and learn to massage out the fluid that builds up on the right side of my neck, but I am still just focusing on resting and getting used to my new life. That seems to be enough right now.